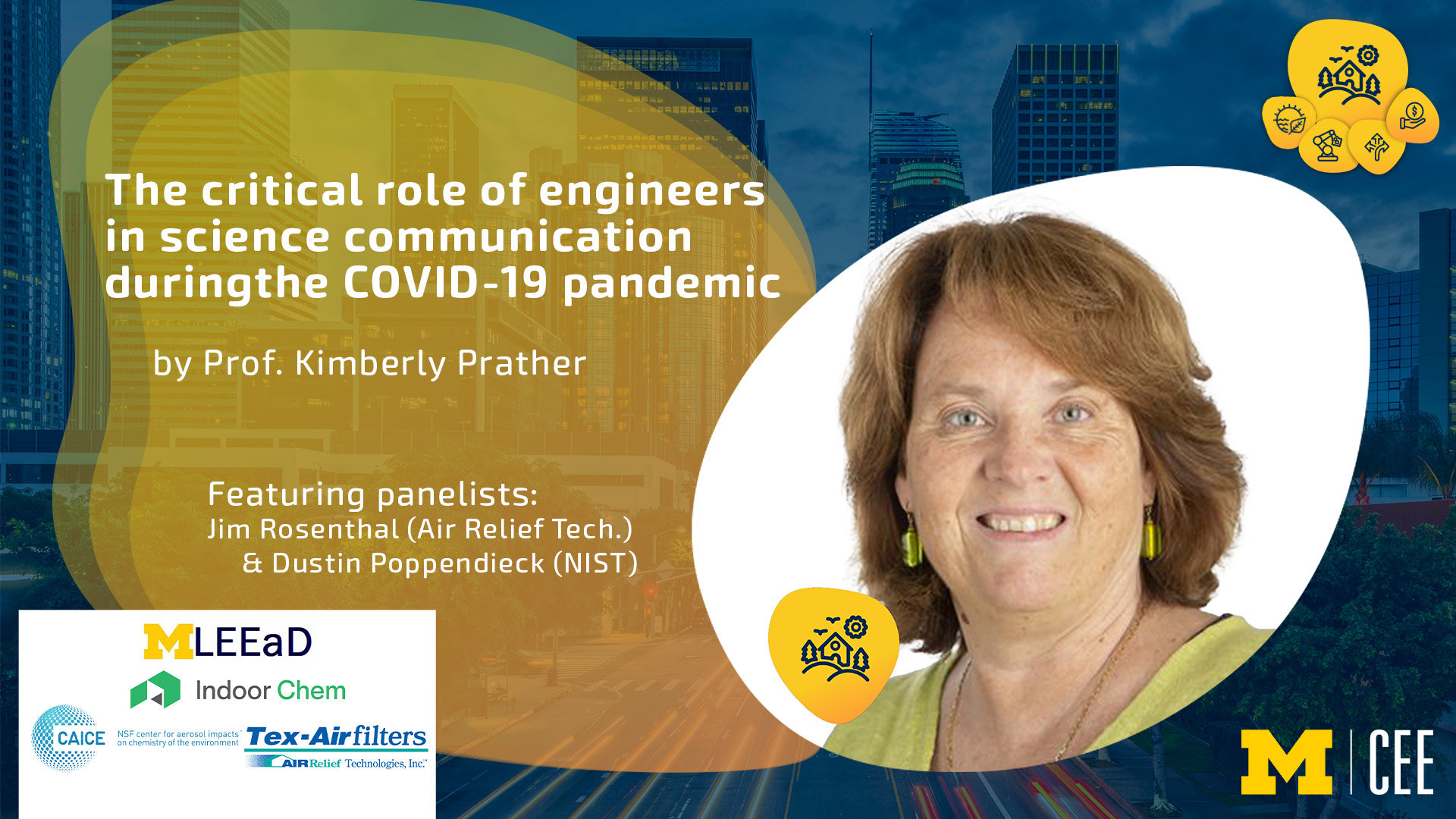
CEE Recaps January 31 Building the Future Webinar
Recording, Q&A and Transcripts from Human Habitat Experience Webinar Featured
Recording, Q&A and Transcripts from Human Habitat Experience Webinar Featured
U-M CEE is providing an extended panel discussion article, consisting of audience questions that were unable to be answered during our January 31, 2023, webinar due to time limitations. This discussion features Dr. Kimberly Prather and panelists Jim Rosenthal and Dustin Poppendieck. We have a link to the video recording of the session, called “The Critical Role of Engineers in Science Communication During the Covid-19 Pandemic.”
Our speaker and panelists graciously agreed to continue their conversation on paper following the initial broadcast, and responded to some additional questions that are included in this article. We have listed citations from the slides used in the presentation. Following this extra content, readers will see the entire transcript from the original recorded session.
From the Extra Q&A Discussion After the Recorded Webinar:
Q1. Would implementing HEPA filtration and Ultraviolet Germicidal Irradiation or Far-UVC reduce transmission of respiratory viruses like COVID-19 indoors? How do these precautions fair in environments where people aren’t wearing PPE like masks? How much would it cost for the University of Michigan to implement HEPA filtration and Far-UVC indoors?
Jim Rosenthal: I am not sure HEPA filtration is a realistic option for U of Michigan. The HVAC systems to run HEPA’s would be prohibitively expensive. The best option at this point is upgrading to MERV 13. Far-UVC is great, but also very expensive at this point.
Dustin Poppendieck: FAR-UVC can produce ozone which can initiate indoor chemical reactions. At this point we still don’t know enough about the process and whether the chemistry is significant enough to impact health and which environments it would be best applied (e.g. dense spaces with high air change rates).
Kimberly Prather: Short term, I firmly believe (based on science) that we should implement standalone filtration (CR boxes or HEPAs) in public spaces. Filtration removes all airborne viruses/particles including allergens, pathogens, and PM pollutants. Adding UV – reduces infectious pathogens but does not improve ventilation or reduce air pollution and allergens.
Q2. What is the most effective way for us to convince President Joe Biden and other responsible elected officials that the (aerosol) COVID pandemic is not over and that masks (a filter/barrier) and MERV /HEPA filters are critical in schools, office buildings, and other indoor venues?
Dustin Poppendieck: Pass as governmental employee.
Kimberly Prather: My view is to start at the state and local levels–show success and hopefully success will grow.
Q3. What do you think can be done to push the WHO to fix their confusing messaging once and for all? It is very frustrating for us (environmental engineer) here, especially in developing countries, when the policy maker, the public, and medical doctor trust what the WHO delineate rather than some of the latest research.
Dustin Poppendieck: Pass as governmental employee.
Kimberly Prather: Not clear what it will take to wake WHO up–will they ever lead the messaging? It is not clear.
Q4. Are face shields with an N95 a good combo or should face shields be avoided altogether?
Jim Rosenthal: Face shields can be good extra protection for the eyes and for situations where there is exposure to larger droplets. But they need to be designed so air cannot pass around the shield.
Dustin Poppendieck: Face shields are good for scenarios with large droplets (like daycares) where they would stop “ballistic” or visible large droplets you can see coming out of a mouth. They do not replace N95s for protection from airborne particles.
Kimberly Prather: Face shields alone are not helpful as they trap aerosols in the breathing zone. If you choose to wear a face shield to protect your eyes from droplets, then you should wear a respirator also.
Q5. Question to Jim Rosenthal: there have been claims that air purifiers based on computer fans provide the same clean air delivery rate as CR boxes, with significantly lower noise level and energy consumption. Do you agree with these claims? (If true, this would require computer fans to be more efficient than box fans by a large factor.)
Jim Rosenthal: Thanks! Some of the new PC fan CR boxes are really impressive. Lower noise, lower energy usage and good CADR. They are not as powerful as CR boxes with regular fans, are more difficult to make and more expensive. They are a step in the right direction but not the final answer in our quest for better indoor air for all.
Q6. ID Docs have built a walled fortress of bad science and established it into public health policy and medical education. They deny COVID is airborne backwards because flawed mask and respirator RCTs don’t show effectiveness. How do we overcome this growing inertia?
Kimberly Prather: The inertia does not appear to be growing. Everyone needs to to push back on misinformation and call it for what it is…why ID doctors continue to push back is unclear given all of the science that shows the virus is mostly spread in tiny aerosols that float in the air like cigarette smoke, not droplets.
Q7. For people that are interested in purchasing a CO2 meter, what are the recommended target CO2 ranges?
Dustin Poppendieck: CO2 meters are great tools to identify ventilation issues in densely populated indoor spaces. They are not as useful in other scenarios (low density). The “ideal” indoor CO2 concentration is highly debatable given lots of variables. Some European countries recommend concentrations below 800 ppm – 1000 ppm as an indicator of good ventilation. However, there are lots of issues (i.e. ventilation can be poor but low CO2 readings initially when people enter). However, if your space has a steady CO2 concentration above 2,500 ppm to 3,000 ppm I think most indoor air professionals would say that indicates the space is poorly ventilated and needs its ventilation system evaluated.
Kimberly Prather: <800 ppm (or <1000 is OK).
Q8. I’m trying to help my mum understand why her air cleaner/purifier that uses ionization & ozone probably isn’t as effective as something like a CR box or device that uses a hepa filter (her primary concerns are covid-prevention and cooking odor reduction, if that helps). Do you have any advice? I LOVE my CR box but the benefits I’ve experienced from it don’t seem to have convinced her… Do you have any advice? Thank you!
Jim Rosenthal: That is a tough one. I have been trying to convince people to abandon their ionizer/ozone products for the past 25 years. My experience is that if someone believes it is helping, they are going to keep believing it – no matter what you say. (But you might turn it down, when you have a chance.)
Dustin Poppendieck: Ozone smells nice, like a lightning storm. So people associate it with cleanliness. Ozone and ionizers add energy to the indoor environment that initiates indoor chemistry which can affect health. Here is a paper that highlights that from this week (https://doi.org/10.1164/rccm.202212-2203LE). As far as showing the HEPA/CR work show a used filter versus a new one. The color difference is what would have been in your lungs.
Kimberly Prather: She needs to know that ionizers and ozone create toxic chemicals that she should NOT be breathing. Simple filtration to take out aerosol particles like respiratory pathogens, dust, smoke, and cooking aerosols is critical and proven.
Q9. In ADDITION to vent/filter, should we also try to prevent contagious from entering certain indoor spaces? Eg, by PCR saliva test to enter/stay (w/ RATs used instead post-infection)? I believe this is used at Davos, some White House events , etc.
Jim Rosenthal: The first step is always prevention. Testing can be a good step. N95 masks are preferred.
Kimberly Prather: Blocking aerosols at the source is key. N95/KN95/KF94 all work well. N95 is the gold standard but less people feel comfortable in them.
Q10. Difficulty arises when CO2 reading does not drop when the HEPA filter is running. How do you communicate that the CO2 is high but HEPA is operating?
Jim Rosenthal: CO2 is a gas. HEPA filters remove particles. They will not affect CO2 levels. But high CO2 levels can be a sign of poor ventilation. That could mean airborne viruses are in the air and need to be removed. The CO2 monitor is a “smoke alarm” not a particle extinguisher.
Dustin Poppendieck: The HEPA filter will not remove gases. So high CO2 but HEPA running means lower exposure to airborne pathogens, but does not necessarily equate to good indoor air quality as gasses can be present.
Q11. 1) How do you reconcile the additional energy needed to heat/cool indoor air w/increased ventilation to obtain the lower CO2 levels that people with CO2 monitors now demand? 2) If institutions claim to be cleaning/filtering the air behind the scene (e.g., in ducts), how can people either confirm/trust these institutions that have been less than honest during the pandemic. 3) How can one convince institutions to install/retrofit expensive equipment, e.g., heat exchangers when they claim “the pandemic is over”?
Jim Rosenthal: I think the first step is awareness of the problem. That is why CO2 meters can be helpful. They inform the building occupants of a safety issue. The feedback from these people can make a difference so that the expense will seem justified.
Dustin Poppendieck: Using CO2 meters that display real time at the entrance to the facility is a great step to building trust between the building occupants and the building operators. Just like health grades for restaurants they build the basic trust needed. An ancillary benefit is they allow thermal comfort issues to be resolved also. As for energy impacts, there is no silver bullet. We need to realize there is an increased energy need to operator our buildings safely. We can address this with heat recovery ventilators to reduce the energy consumption, but also build more renewable, local, distributed energy infrastructure that provides reliability while improving IAQ.
Kimberly Prather: Multiple questions…1) How do you reconcile the additional energy needed to heat/cool indoor air w/increased ventilation to obtain the lower CO2 levels that people with CO2 monitors now demand?
This is nothing compared to illness, death, work and school absences. Linking the ventilation/filtration to PM and CO2 levels saves energy. In the end, it is like running one light bulb–nothing. I have seen this used as a (poor) excuse to not do the right thing.
2) If institutions claim to be cleaning/filtering the air behind the scene (e.g., in ducts), how can people either confirm/trust these institutions that have been less than honest during the pandemic.
They need to provide answers on how they have improved indoor air…what are the CO2 and PM readings? How have they supplemented HVAC (even MERV13 not enough) with standalone filtration systems?
3) How can one convince institutions to install/retrofit expensive equipment, e.g., heat exchangers when they claim “the pandemic is over”?
There are many pubs on this. See Refs below as a starting point.
Q12. If CO2 can negatively impact cognitive abilities and filtration does not reduce CO2 levels, then is it true that filtration is not a solution for poor ventilation?
Dustin Poppendieck: If the space is highly occupied, that is correct, filtration should be used in combination with ventilation.
Q13. Would love a short description of what to look for in a handheld particle counter if there is time.
Dustin Poppendieck: http://poppendieck.com/IAQ/Consumer%20IAQ%20Monitors.html
Q14. My understanding is that CO2 levels above 1000 ppm, and especially above 1500 ppm, are detrimental to good cognition if they persist for considerable lengths of time. Are there any ways to improve ventilation to reduce CO2 in densely-populated spaces (like school classrooms), other than opening windows?
Dustin Poppendieck: It depends on the school HVAC system. There are many different ventilation systems that are implemented in schools in the United States. Higher than expected CO2 levels may simply indicate that the ventilation system has an issue (i.e. turned off, broken damper, bad control).
Kimberly Prather: It is important to bring in as much fresh air as possible through the HVAC system. Recirculating air is not a good idea. If outdoor air is heavily polluted (near freeway, wildfires), then bringing in 100% fresh air coupled with filtration is key.
References from Prof. Prather’s slides:
Derk, R. C.; Coyle, J. P.; Lindsley, W. G.; Blachere, F. M.; Lemons, A. R.; Service, S. K.; Martin, S. B.; Mead, K. R.; Fotta, S. A.; Reynolds, J. S.; et al. Efficacy of Do-It-Yourself air filtration units in reducing exposure to simulated respiratory aerosols. Building and Environment 2023, 229, 109920. DOI: https://doi.org/10.1016/j.buildenv.2022.109920.
Greenhalgh, T.; Fisman, D.; Cane, D. J.; Oliver, M.; Macintyre, C. R. Adapt or die: how the pandemic made the shift from EBM to EBM+ more urgent. BMJ Evidence-Based Medicine 2022, 27 (5), 253-260. DOI: 10.1136/bmjebm-2022-111952.
Greenhalgh, T.; Jimenez, J. L.; Prather, K. A.; Tufekci, Z.; Fisman, D.; Schooley, R. Ten scientific reasons in support of airborne transmission of SARS-CoV-2. The Lancet 2021, 397 (10285), 1603-1605. DOI: 10.1016/S0140-6736(21)00869-2 (accessed 2023/01/31).
Jimenez, J. L.; Marr, L. C.; Randall, K.; Ewing, E. T.; Tufekci, Z.; Greenhalgh, T.; Tellier, R.; Tang, J. W.; Li, Y.; Morawska, L.; et al. What were the historical reasons for the resistance to recognizing airborne transmission during the COVID-19 pandemic? Indoor Air 2022, 32 (8), e13070. DOI: https://doi.org/10.1111/ina.13070.
Morawska, L.; Allen, J.; Bahnfleth, W.; Bluyssen, P. M.; Boerstra, A.; Buonanno, G.; Cao, J. J.; Dancer, S. J.; Floto, A.; Franchimon, F.; et al. A paradigm shift to combat indoor respiratory infection: Building ventilation systems must get much better. Science 2021, 372 (6543), 689-+. DOI: 10.1126/science.abg2025.
Morawska, L.; Milton, D. K. It Is Time to Address Airborne Transmission of Coronavirus Disease 2019 (COVID-19). Clin Infect Dis 2020, 71 (9), 2311-2313. DOI: 10.1093/cid/ciaa939 From NLM.
Prather, K. A.; Marr, L. C.; Schooley, R. T.; McDiarmid, M. A.; Wilson, M. E.; Milton, D. K. Airborne transmission of SARS-CoV-2. Science 2020, 370 (6514), 303-304. DOI: 10.1126/science.abf0521.
Prather, K. A.; Wang, C. C.; Schooley, R. T. Reducing transmission of SARS-CoV-2. Science 2020, 368 (6498), 1422-1424. DOI: 10.1126/science.abc6197.
Sachs, J. D.; Karim, S. S. A.; Aknin, L.; Allen, J.; Brosbøl, K.; Colombo, F.; Barron, G. C.; Espinosa, M. F.; Gaspar, V.; Gaviria, A.; et al. The <em>Lancet</em> Commission on lessons for the future from the COVID-19 pandemic. The Lancet 2022, 400 (10359), 1224-1280. DOI: 10.1016/S0140-6736(22)01585-9 (accessed 2023/01/31).
Wang, C. C.; Prather, K. A.; Sznitman, J.; Jimenez, J. L.; Lakdawala, S. S.; Tufekci, Z.; Marr, L. C. Airborne transmission of respiratory viruses. Science 2021, 373 (6558), eabd9149. DOI: doi:10.1126/science.abd9149.
Wilson, N. M.; Marks, G. B.; Eckhardt, A.; Clarke, A. M.; Young, F. P.; Garden, F. L.; Stewart, W.; Cook, T. M.; Tovey, E. R. The effect of respiratory activity, non-invasive respiratory support and facemasks on aerosol generation and its relevance to COVID-19. Anaesthesia 2021, n/a (n/a). DOI: https://doi.org/10.1111/anae.15475.
Complete Recording Transcript: “The Critical Role of Engineers in Science Communication During the Covid-19 Pandemic.”
Introduction: U-M CEE Interim Chair Yafeng Yin :
Hello everyone. My name is Yafeng Yin. I’m a professor and interim chair of the Department of Civil and Environmental Engineering, University of Michigan. Welcome to the University of Michigan Building the Future Distinguished Lecture series. In 2019, our department completed a strategic visioning process through which we identified five strategic directions. They are, shaping resource flow, adaptation, automation, smart infrastructure finance, and enhancing human habitat experience, which is the topic of today’s webinar. So this direction focuses on advancing new approaches and a solution that aims to enhance user experience in natural and built environments. This is a very exciting focus for our department, and also the profession as a whole. Our strategic vision reaffirms our value proposition to our communities and reinforces our commitment as engineers working in service to society. So to highlight our vision and to formulate a work plan, we launched this Building the Future Distinguished Lecture series, which provides a forum to discuss each strategic direction.
Our goal is to build a broad community network that includes industry professionals, researchers, educators, and students through presentations from leading experts and panel discussions. This series provides new insights and explores a range of perspectives on these five strategic directions. We have had a lot of support to make this vision and today’s webinar come together. We’d like to thank our co-sponsor for today’s event, Air Relief Technology, Inc., Center for ASO impact on chemistry of the environment, UCSD, Indoor Chem, Life Stage Environmental Exposure and Disease Center and the Lifestage Environmental Exposures and Disease Center at the University of Michigan. I’d like to thank the Strategic Implementation Committee led by Professor SangHyun Lee. I also thank Professor Rachel O’Brien, who is assistant professor here at Michigan. Professor O’Brien has agreed to serve as the moderator for today’s presentation and panel discussion.
A few more words on the accessibility of the webinar. We would like to make our event accessible to all participants. Since this webinar will have a live automated caption, a transcript will be available. To choose a viewing option. Click “live transcript” on the control bar at the bottom of your screen where you can show or hide the subtitle or view the whole transcript. I will now turn the session over to Professor O’Brien. Rachel, over to you.
Prof. Rachel O’Brian:
Thank you, Yafeng. I would like to welcome everybody participating in today’s event. Today’s distinguished lecture emphasizes the strategic theme of the enhancing human habitat experience. To give an overview of this theme, I would like to play a two-minute video.
Prof Rachel O’Brian:
All right. During the lecture and panel discussion, I will invite participants to send in your questions using the Q&A function. We will try to get to as many of your questions as time allows. Now I would like to introduce our very special speaker and panelists. We’re very fortunate to have Kim Prather, distinguished professor and share in atmospheric chemistry, UC San Diego, who will speak to us on the topic of the critical role of engineers in science communication during the COVID-19 pandemic. The presentation by Kim will be followed by a panel discussion with our distinguished panelists, Dustin Poppendieck and Jim Rosenthal. Dustin Poppendieck is an environmental engineer at the National Institute of Standards and Technology, and Jim Rosenthal is the chairman and CEO of Air Relief Technologies Incorporated. This brings us to today’s distinguished lecture. Let me now invite Kim to speak on this theme and to give her presentation.
Kimberly Prather:
Okay. Well thank you and it’s an honor to be giving one of these lectures and I would like to thank Dr. O’Brien and Dr. Yin for the invitation to be here today. Well, as was mentioned, I’m going to talk about the critical role of engineers during this pandemic. I’m actually a scientist, but I’ve been sort of, I think I have the brain of an engineer, I think like an engineer. I’m actually in the National Academy of Engineering. I think a lot like an engineer. And I think what I like the best about engineering is just that it’s very solutions oriented and I realize that that is kind of how my brain works. So as I say, I’m an atmospheric chemist.
I’ve developed tools over the years for studying aerosols in the atmosphere and when the pandemic started, I became heavily involved and I will talk about that a little bit today. So a bit of an overview, just quickly. I’ll talk a little bit of background on how the heck I went from studying aerosols and clouds and climate in the ocean and ocean processes to being heavily involved in science communication. I will say that it wasn’t just me, it was a huge team of people including two of the people that are on the panel today. But it was a really amazing sort of grassroots effort of people coming together across disciplines to work together to try and help the public who were highly confused and I’ll talk about that quite a bit today. But mostly I want to also focus on, set ourselves up for a discussion on solutions.
What next? How do we get out of this pandemic, because I’m a believer that we don’t have to just live our lives like this and put up with it. I think there are things we can do. So just a little bit on my background, I am, as was mentioned, I’m the founding director of the NSF Center for Aerosol Impacts on Chemistry of the Environment. I’ve been doing this, I’ve been leading this effort for 13 years now, and it’s sort of morphing from very climate focused to a health focus and basically that’s one of the ways that I got pulled in, but it’s very focused on aerosols and how aerosols are produced and how they move through the air and sort of aerosol science as a whole is something that started out in the engineering community. So let’s just step back and think about just to touch on where we were and where we are.
Sometimes they’re a little bit too much, the same given all that’s happened in between. But the bottom line is that early messaging, how does this virus get transmitted? It’s through the air. That’s the simple answer and that’s actually what the WHO World Health Organization stated clearly on February 11th, 2020. But within five, 10 minutes after a quick little side conversation, he came back and said, “It’s not airborne. I shouldn’t have said that.” And they took it back. They have a tweet. They put up a tweet, which is still on Twitter, which a lot of people are pushing on like, “Why is that still there? This is misinformation. They claim they can’t remove tweets, but they do.” But this one is, you can still find it. And so this kind of is at the heart and soul of frustration. I have no other word to describe to many of us that the public is confused and rightly so because they hear different things.
But the fact is this particular virus and actually many, many viruses, there’s a huge airborne component to them. And it’s something that once it’s acknowledged, once people understand many of us have been delivering the message, then it can be easily fixed. So again, adding to the confusion, they say that it isn’t airborne, but it’s definitely borne by air. I mean, that’s the kind of information that has been out there and is sadly still out there.
So where did I come in? So I was just quietly running a center and along came a reporter who asked me if I think that if the virus that causes COVID-19 could travel more than six feet. And what comes to mind is, I fly around the world through clouds. Aerosols can go all the way around the globe in about two weeks. So yes, I do think that aerosols can travel further than six feet.
And so that led me to write a paper with an infectious disease doctor here at UC San Diego and a colleague in Taiwan. And basically we just sort of stitched the pieces together. This virus is getting around mostly in aerosols. It’s being released by people who are just simply speaking, singing. They don’t know they’re sick. And so that is the sneaky side of this virus and how things had unfolded at that time. So this paper ended up being incredibly cited, downloaded. It’s the most downloaded paper in science history, I’m told. It really sort of resonated with people. But this was back in, I mean I wrote it in May 2020 and here we are.
So then that wasn’t enough. I just sort of want to give you a flavor for the different little things we tried. But after some workshops by the National Academy, we basically said there was this arbitrary break that’s been there for a long time that separates aerosols and droplets, and I’ll talk more about it.
It’s five microns. And so we basically said, “No, that break should be 100 microns. Things that are up to 100 microns can go further than six feet. And then finally we wrote a review article which said it’s not just SARS-CoV-2 that’s airborne and can go further than six feet. It’s all of these different airborne viruses. All of them have some airborne component with a motivation being that if we can protect ourselves and protect everyone from this one virus at the same time we’re protecting everyone from all of these other illnesses. It’s a huge, it’s no-brainer from a public health perspective to do something about getting these viruses out of the air.
The other thing we did, this was written with people that Trish Greenhouse led the charge on this paper. We stitched together, I mean, all evidence pointed at way back then. This is 2021, but even as far back as 2020, everything pointed at airborne. These are 10 solid reasons that all point to airborne. And so again, we still had resistance. So my main message from the beginning has always been again, solutions oriented and optimistic that once we acknowledge it’s airborne, we can fix it. It’s a fixable problem. We can clean the air just like we filter our water, we remove pathogens from water before we drink it. We’re exposed to far more air during thousands of times, more air during the course of a day. We breathe 22,000 breaths a day and we’re perfectly content for some reason to continue to breathe in pathogens and other harmful pollutants.
So anyway, this is sort of where Twitter came in and this is what I would say is the good side of Twitter. There is a good side. It brought together many of us, including those of us as part of the seminar, met through largely through Twitter. And so it’s just sort of this group of people spanning from doctors, lawyers, general public, people who just had a general interest in the problem. We came together and started pushing sort of the information out there to help the public because the public was so desperate for honest, straightforward information. So this is just a little sort of step through time.
We basically. I’ve met many of the people that I only knew through my computer. These are shown here. We took one of these Corsi-Rosenthal boxes that I’ll talk about. Today we took it to the White House. This is Jim Rosenthal, who you’ll see later. Don Milton. I met the team, Team Airborne, this is the founder of Team Airborne here. And I met her in Bern and they brought a bunch of very kind notes to me and even made me a 3D printed fact, COVID is airborne and this is a doctor that was heavily involved that I met in DC. I mean, I could put up many of these pictures, but kind of everywhere I travel now I’m finally getting to meet all the people that we’ve worked so closely with over the last few years.
I was kind of curious from the standpoint of your search on airborne transmission, how much of a role have engineers played? This is one way that I kind of peeked to see, and these are all the different categories of basically the different types of journals where this term, airborne transmission, has appeared. And so you can see that basically engineering’s everywhere. There’s public environmental, occupational health, and one could argue that some of those are engineering journals, but engineering infectious disease is here. It’s the third ranked one pretty far down, but it’s there.
But it’s basically largely been driven… I mean it’s air movement. And so it’s just understanding how aerosols move through the atmosphere, how they move through a building, how we can protect ourselves from ventilation and filtration. This is right at the heart of engineering and engineers have played a major role in this.
So the other thing, just sort of to give you a flavor in addition to writing papers, in addition to going to Twitter, this is Lindsay Maher, speaking of an engineer. I met her. I knew her before, but I’ve gotten to know her much better through this. We’ve worked together on many different workshops and this is our efforts through TV. Dr. LaPook, who’s the CBS chief medical correspondent, has become a good friend of mine. He has been a huge advocate for COVID as airborne and helped us in getting the word out. We’ve done, I don’t know how many different media interviews to try and get it out again to the public.
There’s also the National Academy of Engineering and Sciences and Medicine. NASA has done multiple workshops, multiple, I mean multiple, multiple. They aren’t even all listed here. Again, in basically the main conclusion of the scientists at these workshops and in these reports, it’s no question that this virus is mostly transmitted through the airborne pathway. And you may say, “We all know this. Why are you saying it again?” And I get that question oftentimes. But when you walk into a business, what do you see? Do you see filters, air filters, or do you see hand sanitizer? And I know what I see. I see people with no masks. I see people while they’re wiping their hands, sanitizing their hands, sanitizing their shopping carts and no mask. So there’s still confusion out there, unfortunately.
This is actually taken from a National Academy workshop. It’s a drawing that came from Lindsey Moore, actually from one of her kids did it. And it’s been used over and over, but it sort of gives the major modes, which is the focus has always been on droplets. And I’ll just say, and Dustin will back me up on this, droplets drop, and that was the fixation of the medical community for the last at least 50 years. And so that’s where the six feet came in. But there’s not that many droplets that are produced. There’s probably 100 to 1,000 more aerosols for every droplet when you’re speaking that are produced.
And those aerosols float in the air like cigarette smoke. And if you’re in a poorly ventilated indoor space, they can build up just like cigarette smoke as well. And so being six feet away is not enough. Yes, it’s worse to be close because it’s much more concentrated up close. But the bottom line is, aerosols float while droplets drop. And so sometimes there’s still debate. They call long-range aerosol inhalation. There’s terminology that’s airborne and short range is not crazy terminology things. It doesn’t matter how far the virus travels. You want to protect yourself against inhalation because it’s in the air.
So should it be a surprise? No, we knew SARS-1. Where would you look? So SARS-2, look at SARS-1. SARS-1 we know was basically this is the Amoy Garden situation with buildings where it actually traveled between floors of a building and people on the upper floors got hit with it higher and they figured out that it came from outdoor transport of raw sewage.
And so again, it’s not… At that time they said it was airborne. And one of the major conclusions of their looking into it was they said that the most important thing you can do if something like this ever happens again, is to exercise the precautionary principle, which means don’t wait until you have all the science lined up and perfect. If there’s any chance that something could be transmitted via a certain pathway in this case the air, then you should do something to protect people against the potential for that pathway. We did not do that. But we’ve known even before then. This goes back to Florence Nightingale. This goes way, way back. This was published in 1863. She talks about her wishes that people were forced to bring in fresh air, talks about the concern about schools being crowded and the chance of transmission. So she was a nurse and building engineer as they titled her at the time.
And so this should not be a surprise and it should not be something that we are still having to talk about at this point. So a couple of questions. Where did the precautionary principle go? We know the virus is airborne. There is zero question about that. And so why has there been such hesitancy to use the word airborne? I get asked that question more than any other question and I can only speculate someday maybe we’ll know. So you might say, “Okay, it’s clear, it’s done. People must get it now,” and here’s more evidence that’s not the case. This is a tweet that just came out just a month ago from a pretty well known infectious disease doctor up in Canada. And she basically says, in complete honesty, “I strongly suggest engineers shouldn’t tell ID docs and infection control docs how to manage PPE, personal protection equipment and outbreaks in hospitals.
So here we are, this is part of the problem. Engineers look at airflow, they look at how aerosols move. They designed the masks. They designed the ventilation system. So why are they somehow not supposed to be commenting? Another thing that’s gone on is from a medical doctor perspective, what do they believe in? Why are they so adamant and not wanting to pay attention to direct measurements? They do these things called RCTs, random control trials. This just came out. It’s shocking to me quite honestly that you do a random control trial on masks. There’s some serious ethical issues. The design of the studies is seriously flawed actually, because one thing they’re looking at is sort of the protection of the individual and wearing a mask and wearing it properly and wearing the proper mask, which that’s part of the problem a lot of people don’t know.
They wear these baggy blue, we call them masks, thinking they’re fine, they’re not. But it’s more than that. Masks in terms of infection control, the number one thing they do is source control is what we call source control. They block it at the source. You never want the virus to get in the air in the first place. These studies have no way to assess that aspect. And so they are missing the point.
So just to go at what’s the basic data, and to me this is one of the most shocking things of the entire pandemic. Basically there’s these things called aerosol AGMPs aerosol generating medical procedures. And what they are, they look at a number of aerosols that come out from different activities and these AGMPs are intubation and things like that that are listed over here on the right.
And then if you compare those though, aerosol scientists came along and said, “Well, let’s look at how many aerosols come out of a human that’s just talking or exercising or shouting or coughing.” A lot more come out of a human just from simple activities. And if that person is infectious and doesn’t know it or does know it, those aerosols actually contain the virus, right? And so it’s sort of the thing that’s really crazy is you still hear doctors saying, “We wear 95s, the really good respirators whenever we’re doing AGMPs.” But the point is is that these basically in the case of a doctor dealing with people that potentially have it, and again, we oftentimes don’t know the person’s sick, what do we give them? We give them a surgical mask. I can’t tell you how many times I’ve heard stories of people going to the hospital or to a medical facility and being told to take off their N 95, the ones shown over here and put on a surgical mask, backwards.
And so we give them the poor respiratory protection where most of the aerosols are formed and we give them the best respiratory protection where there’s not as much. And so we argue this is a paper by Wilson of 2021. We argue the risk of aerosol exposure is underappreciated and warrants widespread interventions. Again, this is from 2021 and we’re still stuck.
So there’s a really good paper I’ll just quickly mention. I want to make sure that I’m staying on time so we have time for discussion. This was led by Jose Jimenez from University of Colorado. It goes into sort of the theory of how diseases are transmitted. There was a period where they realized it was air, it was in the air, viruses were in the air. They called it miasma theory. But then it went back. There became resistance to airborne. And now we’ve seen the shift back to things being in the air and being accepted as being in the air. It’s quite an interesting paper if you’re interested in the history of these things.
The other thing that came out was a paper or a Lancet study sort of looking at what have we learned? How can we avoid such messes in the future, for lack of a better term. How could we avoid pandemics in the future? One way is to actually clean the air, indoor air in particular. And so one of the major findings of this commission report, which just came out in the fall, was WHO acted too cautiously and too slowly on several matters. One was in endorsing the public use of face masks as protective gear or respirators and to recognize the airborne transmission of the virus. And I will still say if you do a search in Twitter and you look for the word airborne and WHO, they still are avoiding the use of the word airborne.
They will tell you to ventilate, the importance of ventilation. They’ll tell you to wear masks, but they still will not use the word airborne for whatever reason. So if we think about where are we in terms of understanding air quality, again, a very engineering problem. We basically have focused all like the money, the investment has gone into cleaning outdoor air, which is a good thing. People sort of think about [inaudible 00:25:46] air is much safer than indoor air because things are more dilute. You can’t tell that here. Outdoors it’s pretty darn dirty. And air pollution is responsible for killing about an extra 7 million people per year. The other thing is that 70 to 75% of the people globally live in areas where concentrations of PM, particulate matter exceed the WHO’s limit of 10 micrograms per cubic meter are breathing unhealthy air, that’s outdoors.
So we’re very, as a world, as a globe, we’re very fixated on outdoor air. What about indoor air? Well, we spend 90% of our time indoors. And here’s the pun. There are these two things on the left to sort of show the pie chart and then time of day to show how little time we actually spend outdoors. Most of our exposure to air pollution and to any sort of respiratory disease, it’s going to come indoors where indoor air pollutants can be two to five times higher than outdoor levels. They can be over 100 times higher routinely indoors because things just build up a lot. Most places do not have good ventilation. And so basically what we should be worried about is our indoor air and we just, for some reason it has been neglected. I will say that is, I don’t know if there’s a silver lining in the pandemic, but I will say this pandemic has drawn attention to the type of air we breathe and the poor air we breathe indoors.
So there’s been a shift, a big shift. This was a paper led by Lydia Moroska, which was to start thinking about better design for buildings. How do we combat these high pollution levels inside and start thinking about things like air changes per hour. I think my neighbors now know the term air changes per hour. Homes, it’s about one air change per hour, which is very low. Hospitals get up to about 12 in areas where they’re worried about respiratory protection. So that means basically it’s every five minutes or so you get, in theory, sort of fresh air. In schools, it’s less than two. It’s much less than that in reality in most schools that people check. Yet, parents will go, “I want to make sure my kids are breathing clean air at school.” And what do the administrators tell them most of the time, “It’s fine. We’ve got it covered. We’ve cleaned the air.” That’s sort of those kinds of hand waving answers.
So we went in. I actually helped the San Diego Unified School District, which is one of the largest ones in the United States. And we were successful through Delta. It got more challenging as Omicron and the other variants came along. We would argue that we just should never, if we nipped it in the bud, we wouldn’t have had these variants that were so much more difficult to control. But we were able to measure things. This is engineering 101. You can actually measure particles, how many particles are in the air. You can measure ventilation, the level of ventilation using this little CO2 meter that I show here.
We actually had in the classrooms, they had these little QR codes that the parents could take a snap of and then go learn. Because a lot of times parents and teachers and even kids, they don’t really understand why these things are there. Why is the filter running? Why are the windows open? Why is the door open? So there’s just all kinds of ways that we can actually go into improving indoor air quality. These are sort of listed here and I have a feeling that will come up in the discussion. This is something that’s just sort of missing in when… The implementation part has been lacking is what I will say. So we can again talk more.
But again, when you increase ventilation, you decrease CO2 and it’s been shown repeatedly that that increases attendance, attention and test scores. So it’s a win-win all the way around including the public health side. So we have Jim Rosenthal here and he has been incredibly helpful. He and Corsi are also looking at sort of making these little boxes, these handmade boxes, which I’ve talked so much about, people think that I have some sort of vested interest. I don’t, other than protecting people’s health.
They work incredibly well and in fact they outperform HEPAs. And so I like them because, and I push them because it’s an equity issue. More people can have access to these. They cost, if you build them yourself, takes about, I don’t know, between 15 and 30 minutes depending on how many you’ve built. You tape them together. We can talk more about it. It costs about $70. Some people say they look ugly. I think they’re beautiful when I think about the job that they’re performing. This just shows sort of how simple they are to put together, duct tape and you’ve got the box. They cost way less. They can be quiet. Most people don’t know that it’s best to just run them on low so they can supplement up to, and they can get you up to 12 air changes per hour. We’re getting near hospital level air changes per hour by sticking a couple of these in the classroom.
And again, thinking about them, what are they doing? The simple way is they’re breathing in air at 2,000 times the rate a human can. So they just filter the pollution, the wildfire smoke, the allergens, the respiratory viruses. It goes into that box instead of your lungs and they can be cute. And so there’s all kinds of designs that are all over the web. It’s been fun to watch people build these.
So the last thing I’ll say is, do they work? The most recent paper that just came out talking about how they reduce risk and lower exposure levels as shown here, and basically I’ll just give you a nutshell. They took a source as shown here, a little map of people and you can see that they basically released aerosol at one location and looked at the exposure.
What they found is with just HVAC alone, yellow has high levels of particulate matter or aerosols, 29.4, which it’s high. And you can see that with just HVAC it stays high. They started playing around with putting one in the front and then one in the back, one in basically different, started at different sort of speeds, high and low. And then finally purple is really low concentrations and you can see they put one at the front and one at the back. So two in a room, particles are gone. So it’s hard to surprise anybody by saying, “We took out the aerosols in the air so they aren’t there to be inhaled.” What does that do? It reduces the chance of you inhaling them and getting infected. You can see that the best scenario in sort of overall exposure was going from looking at… They compared unmasked and masked. And so clearly the best is to run two of these and have people masked. But I would argue that as time goes on, if we really clean indoor air environments, we won’t have to have the masks, as people ask me forever?
We can actually clean indoor air. It matters that we do that first. So what would it cost? Depending on how much you estimate, if we want to put one in every school in the US it works out to be about $4 per student per year. Basically, it’s a huge equity issue because sometimes people will say, “Well why don’t you just open the window?” But there’s people that live in places that have such poor air quality or regions that they can’t open their windows and their doors. So these would allow the supplemental aspects will allow everyone to reduce asthma, allergies, sort of everything that you can think about. And again, just the overall ventilation concept of lowering CO2 levels, I should say, will improve cognitive function. So question is why not? And we’ll have more discussion about that I’m sure.
So SARS-CoV-2, the virus that causes COVID-19 is airborne. And we really still are pushing, trying to get the public health agencies to make a clearer message. And the public deserves to understand why. It’s been shown that if people understand why they’re told to do something, they have a greater chance of actually doing it.
We’ve known since back in again long ago, here’s just a picture of 1918 kids outdoors in class. This is their outdoor classroom during the pandemic we had over 100 years ago. And so everyone in the public, little kids understand how these filters work. And again, also just understanding why the more layers of protection you use, the safer you’ll become. In addition to saying what to do, it also tells you what not to do. Not to be the one when you’re speaking, to remove your mask, not to be indoors in crowded settings. When the circulation patterns are high. Plexi without a mask underneath sort of plexi barriers can trap aerosols and actually make it worse. Think about if you were on the other side of a plexiglass barrier from someone who’s smoking. Do you think you’d smell it? Of course you would. And it can actually make it again, make it worse.
People wearing these face shields with no masks can get aerosols trapped inside. That’s not a good thing. Distance is a good thing, even indoors. Singing, the more you yell, the more you exert yourself, the more aerosols and ventilation. I’m just so much more sensitive to ventilation. I take my 2 cents everywhere I go in public places. So we’re not done yet with this pandemic. I hope the more people that can get educated and think about these things and spread the word, the sooner that we’ll get there.
So short term filter indoor air, add these filtration devices. Who cares if they use duct tape. You can make them as nice as you want. Longer term, there should be an indoor air standard, just like we have one for outdoors. Other ideas? This is a talk by Paula Olsiewski and she talked about how we really need a task force to sort of think about schools to protect our kids and what could we do? For the longer term, what should we be doing? And I hope this is something that we can have a conversation about. So I’d like to thank everybody for your attention and I look forward to the discussion.
Prof Rachel O’Brian:
All right, thank you so much. That was an absolutely amazing presentation and a very inspiring talk. So at this point I would like to transition to the panel discussion. So I’m going to invite our panelists to unmute themselves and to turn on their cameras. And while they’re doing that and we’re getting everything set up, I am going to do some brief introductions again for anybody who joined us a little bit late. So we have three panelists here.
Our first panelist is our speaker and that is Professor Kim Prather. Kim Prather is a distinguished chair in atmospheric chemistry and distinguished professor at the University of California San Diego. She received her PhD from UC Davis and at San Diego her research is focused on atmospheric chemistry with a particular focus on aerosol particles. During the pandemic, Professor Prather has been the leading voice in airborne transmission as well as the methods that we can use to protect against the spread of Adenovirus. And she’s received numerous awards throughout her work. I’m only going to be able to cover a few of these.
So she is an elected member of the American Academy of Arts and Sciences, the National Academy of Engineering, the National Academy of Sciences, and the American Philosophical Society. And then I just received news that this morning she also found out that she has been awarded the Gustavus John Esselen Award from the American Chemical Society for her science communication efforts. Our two other panelists are first, Jim Rosenthal, who is a co-founder of Air Relief Technologies Incorporated, which is the parent company for Texas Air Filters. So he has been in the air filtration industry since 1997 and he is certified air filtration specialist from the National Air Filtration Association. He’s been a leading voice on air filtration methods to improve indoor air quality during the pandemic.
And then our third panelist is Dustin Poppendieck. Dr. Poppendieck is a building environmental engineer at the National Institute of Standards and Technology or NIST. He received his PhD in civil environmental engineering from the University of Texas at Austin. So he is a fellow of the International Society for Indoor Air Quality and Climate, and he has been investigating indoor air chemistry for multiple decades. So at this point I’d like to start with our questions, assuming we’re all set. And I’m going to start with some of the ones that were submitted in advance. We had a number of questions submitted, so this is kind of a summation of a group of them, but I’d like to invite our panelists to give us some general comments around the numerous questions concerning air cleaning technologies and methods like ventilation and addition, tie that into regulations and think about how we can protect ourselves and how we can actually move forward to get beyond this pandemic. So to open the floor to our panelists. Jim, if you’d like to start.
Jim Rosenthal:
Sure. Great presentation, Kim. That was really, really well done. And we have known each other for two years. I needed to join Twitter and follow Lindsey Maher and did and wound up making some wonderful friends who are coworkers on this indoor air issue. I think a few things that stick out. One is that we need to focus on measurement. We need to understand that if we don’t measure it, we’re never going to be able to fix it. So Kim presented this little CO2 meter. I think that’s a wonderful, very effective device, but there are other things, particle counters. She showed that also. I think that that’s the first step. If we understand what the problems are, then we can start making some progress on solving them. The other thing is we need to make sure that we have equity, that this goes throughout the society.
It’s not just certain people who can afford certain things benefit from the work we’re doing. And that’s why I think this Corsi-Rosenthal box is important and it was started as an open source thing. Nobody’s making any money on Corsi-Rosenthal boxes. It was the right thing to do and we’re so happy that people all over the world have been using this technique to lower their level of infectious dose. So it’s been a good journey. So those are some things we can do. I think we can expand this Corsi-Rosenthal box idea for $70. You can make them. Put two in a classroom and dramatically decrease the transmission of disease in a classroom, plus protect you from wildfire smoke and allergens and all the airborne things that are in a classroom. Thank you.
Dustin Poppendieck:
Should I go?
Prof Rachel O’Brian:
You’d like to, yeah, jump in.
Dustin Poppendieck:
Yeah, I just want to start off with, yeah, Twitter, joined me with this community. And so there are some positives. Also, I am a federal employee and what I say for the rest of the seminar is my own views, not views of NIST or the federal government. I think we need to step back and take a look at water and how water regulations evolved over the century. Environmental and civil engineers have saved more lives than all the doctors ever have in history in just 100 years of water treatment. And how did we do that? Well, first of all, we defined the problem with John Snow finding the broad street pump and actually took years to maybe some would say decades to get a consensus on waterborne diseases. Once we had that, then we developed the technologies, the treatments, the sand filters, the disinfections to mitigate the waterborne diseases.
And then eventually we moved on to regulations and we actually have regulations in water for what the biological levels can be, what the chemicals can be. And we didn’t start where we are now. It’s really important to remember that it took decades to get all of these things. We didn’t start by saying that we have to measure PFAS in water. We started by saying the BOD needs to be a certain level. And so now consumers don’t think… And then we got to the point where we’re reporting annually. There is a report, everybody knows what’s in their drinking water. Once a year you get a report on what is in there. Consumers don’t think about what’s in their water, they just know it’s clean. But they also know if they’re educated enough not to go into muddy puddles and drink that water. And we need to do that with air.
So in air, we’re still at the problem treatment stage, we’re still trying to figure out how do we define the problem? What is the problem? What are all the technologies that will work, what technologies won’t work? And in air, we have a different way that we go about these things currently. We have non-regulatory bodies that are bodies for advising, for building construction standards like ASH rate. And that gets incorporated into some local regulations. But what we really need is a state and local and federal standards because engineers are really good at designing for a known problem and targeting a known regulation. And until we have that, we’re not going to get the movement on the air quality. So we need that driving force that we can actually design to. And the real critical point that I think needs to be thought about is it doesn’t need to be perfect.
As I said, we didn’t start with regulating PFAS and water when we talked about water treatment. We started with the low-hanging fruit and what we could achieve immediately. And we started improving the really bad things and slowly we built up over time to get excellent water quality. And we need to do that in air quality. We need to start finding these low hanging fruit where we can get consensus and regulations. Personally, I don’t really care if a building’s 800 or 1,000. I care if that building has a PPM of CO2. I care if that building’s at 5,000 PPM. And we have schools that are at that level. We have kids who are trying to think in buildings that have 4,000 PPM of CO2. And I think we can start creating regulations and standards for performance-based metrics that people, [inaudible 00:44:24] I think that’s where we need to start moving towards.
Prof Rachel O’Brian:
Thank you. Kim, do you have any response?
Kimberly Prather:
I think I had my chance to answer that as I was going. So let’s try and get through more of the questions because I see there’s quite a few.
Prof Rachel O’Brian:
Yeah, there’s a lot of these coming in. So for our next question, I want to go back to this idea that’s been raised a couple of times. This idea of CO2 levels and CO2 monitors. Can I get some comments on the actual use of this in buildings, right? So what about perspectives for having these visibly displayed so that everybody can get kind of an instant read on what the CO2 levels are? And then how would people think about this if they’re in different environments? If they, say, have an air purifier, like a Corsi-Rosenthal box in the room, how does that impact their interpretation?
Jim Rosenthal:
Well, the CO2 meter is really the alarm. It’s the smoke alarm. It tells you that there’s not ventilation. Yeah, right here. It’s 550 in my office. It gives you an idea of when there’s a problem and that you need to start working for a solution. You need to either ventilate more, filter more. It gives you great data that gives you just a better environment if you listen to it.
I’m avid, go on an airplane, always take my CO2 meter and it’s really fun because I get all kinds of looks and mostly dirty looks. But when you enter the airplane and you’re there during the entrance period, a lot of times the HEPA filters are not working and the CO2 level easily goes up to 2,400 ppm. That means about 5% of the air you’re breathing at that point is coming out of somebody else’s lungs. It’s just outrageous. And I guarantee you, if we were in the airplane in front of each section on the front wall, if you had the CO2 number, if it was 2,400, we’d be doing something about this. We would be able to solve this problem if we had that information out there.
Go ahead, Dustin.
Dustin Poppendieck:
So I’d see CO2 monitors. I see three major things. Number one is transparency. It’s just like health grades. You’re not going to go into a restaurant that has an F on a health grade and has found a rat in the back on the thing. And so we need these things and to provide transparency to our densely occupied spaces and schools and other commercial spaces. It gains occupant trust. Another important thing is that anytime you have these monitors, they actually measure temperature also and relative humidity. And it’s really important to remember that IEQ can also be IEQ, indoor environmental quality. And people respond to thermal comfort. If there’s a thermal comfort problem, people are going to complain about it. So when you have the ability to measure CO2, we’re going to need to tie that into thermal comfort because if we can get people to buy in thermal comfort’s important, then we can also tie it into CO2.
The next big thing with these CO2 monitors is the responsibility. It shouldn’t be the responsibility of the occupant to address high CO2 levels. It should be the responsibility of the building operator. People who are using indoor spaces are not there to constantly monitor a CO2 monitor and open and close windows and things like that. These people who operate the buildings need to be responsible. And so these AirNet sensors are great, but we need things that are logging real time and somebody can monitor from a remote space so they can actually see where the problems are. And that’s where some of these school districts that are applying these monitors that can look at classrooms broad spread and see where the problems are from both the thermal comfort and a CO2 are really great.
And the last thing I want to address is CO2 monitors are… Despite the fact that I love them, are not the silver bullet and neither are air cleaners. CO2 is really only good for densely occupied spaces. It’s not going to tell us whether air quality is good or not in spaces that aren’t densely occupied. My office, I have two people in it and now I could have a really bad chemical in here that got dragged in from the lab this morning. That’s not going to be represented by CO2.
Also, air purifiers, if you’re going to try and get a credit for having [inaudible 00:49:07] purifier for a high CO2, you need to be aware that that really needs to be addressed by a professional if we’re going to get that credit because you can have people put in an air purifier, one, may not be on, two, it may be way undersized. And three, air purists can sometimes, depending on the type of air cleaning technology, negatively impact other parameters of the indoor air quality.
Air cleaning is not just biologicals, it’s not just air particles and viruses, but it’s also chemicals. And we need to be aware of what we’re doing from a chemicals’ perspective. And so air cleaning, most air cleaning technologies really only address particles. And so we need to make sure that we’re talking about air cleaning, we realize that there’s no real silver bullet. We have to take into account ventilation, we have to take into account particles, air cleaning things. But it’s all going to be a combined effort. There’s no single thing that we can do, but we can use CO2 monitors to identify those really poorly ventilated, densely occupied spaces and get people to act on them if we have appropriate regulations.
Kimberly Prather:
I’ll just quickly chime in, just I agree. The comments are so good and I just want to make one point, because there’s actually, I’m kind of looking at the questions in the chat that are coming in and trying to think about it. I mean there is confusion over the CO2 sensors. They’re simplest, most available thing that we have, but they only get you so far. And a lot of times people get really confused. Even on an airplane when you see it at 3,600 ppm, that looks bad. We want it to be what number do we want? We’d like it to be like outdoors which is what, 420 but less than 800, I’m pretty comfortable. It just tells you you have fresh air is basically what it tells you. But if you have filtration running as airplanes do, it’s not going to change the CO2 level.
So sometimes people get confused by that. And I get asked that question quite a bit, which brings me to my final point, which is, the tools exist to clean indoor air. The tools exist to measure indoor air. We have everything we need. The science supports what we’re saying. We need to do something. And so what I see is implementation is a big problem. And part of that is just the education component. I can’t tell you, we have filters here at UCSD we have Corsi-Rosenthal boxes in all the main large lecture halls. I won’t lecture if I don’t have a CR box next to me or between me and the audience. And even then I still will wear my mask when things are bad. But I can’t tell you how many times I walk in that room and that box is unplugged.
And these are professors that should know better, but there you have it. But in schools it’s even worse. And so one of the things we did in San Diego Unified was we ran these particle counters around and kept those in different rooms that had poor ventilation. And then the facilities people would see if one started getting really super high on particles, which is where the virus is, and they would go find, inevitably someone had turned off the box. But people turn them off because they don’t know that you’re supposed to run them on low and then it’s fine. So there’s just a lot of education and a lot of steps behind. It’s not the lack of science or measurements. Those are the points I want to make. It’s implementation and education that we have to somehow do better on.
Prof Rachel O’Brian:
Great. Thank you so much. This is a wonderful discussion. So I want to bring this. We have time for one more question. I want to kind of bring this back to the overall theme of this talk, and that’s communication and really trying to get this message out, but communicating on multiple levels, so communicating across different fields, but also for scientists, but non-scientists and non-engineers to be able to communicate the needs. And so any recommendations that our panelists have for how people in the audience or any of us can start to try to facilitate these types of changes in our spaces?
Jim Rosenthal:
Well, it’s communication. People forget this, but communication is repetition and being able to repeat the message over and over is very important. And then it’s education. I mean, how do we bring this to the elementary school students? How do we make sure that people understand things like what a PPM is? And in that regard, I’m actually somewhat encouraged by the fact that we are smarter today than we were three years ago.
The general public knows much more about air filtration, about CO2 levels, about all kinds of different things and it’s not the majority of people, but certainly there are a lot of people that understand what needs to be done. So I think it is repetition, having the message, repeating it. One thing we’re doing this Corsi-Rosenthal box idea, one, it’s not a product, it’s a movement and it’s all over the world. And we have started a foundation called the Corsi-Rosenthal Foundation. And the idea is to put together class programs that go to different schools all over the country and make sure that these things are taught and learned. This is the best STEM project that I’ve ever seen and it teaches so much. And I think if we start young and make sure that the kids learn about this, a lot of times they’re the best educators. So that’s what I think needs to be done.
Dustin Poppendieck:
I’ll go back to what Rich Percy 20 years ago said, we need more sociologists than psychologists in the field studying indoor air. And I’m really a novice at how to convince other people on what to do. And from where I sit, I see the problem with indoor air quality is somewhat related to not wanting to change an inertia and finding reasons not to change. A lot of it is people see their side of things as morally right. And you can look at the recent debate on gas stoves. It becomes a moral question of what your morals are versus somebody else’s morals when all I want to say is cast stoves make your indoor air quality worse. And so how do we communicate that in a way that benefits not just a few, but the masses?
And to me, I think focusing on the improvements of individuals’ lives as opposed to big picture things, focusing on improvement on your financial situation, your health and things like that, where you can see immediate benefit impacts of increased performance in your schools and things like that. I think that’s one of the big picture ways I would go about it.
Prof Rachel O’Brian:
Thank you. Kim, do you have any final thoughts?
Kimberly Prather:
Not on that question. Okay.
Prof Rachel O’Brian:
All right. Well then in the last minute or two, I’d like to finish up with any final thoughts from our panelists on any of the topics that were raised today in terms of communication and education and really just this question of indoor air quality.
Kimberly Prather:
Okay, I’ll go. Yeah, I mean, just first of all, I want to, again, thank you for holding this. I see there’s a lot of interest in it. It’s nice to see so many people who care and we just have to get the word out. I keep thinking the word has somehow, and one of the things I’m doing, I didn’t mention, but there’s questions about how we do this and I sort of started at the big level of thinking WHO, CDC. And there was not enough movement there. The White House, but now I’m sort of working with the state of California, which has led… I sort of convinced them that we led the charge in cleaning our outdoor air. So why don’t we lead the charge in indoor air? So I believe in little levers and I’m hopeful that we can sort of pass some, and I know there are states that are doing this, that are starting to go after this clean air standard. So that gives me lots of hope.
I mean, I keep hearing, “Don’t we want our lives back?” Of course, we all want our lives back and I think we can have them back. We just need to… I’d feel more comfortable if we would clean indoor air first and then I’d be, again, I’d be more content on getting my life back as well because this has been dragging on way too long. So that’s my last comment. Thank you and thanks again for having me.
Prof Rachel O’Brian:
Thank you all so much. That was an amazing presentation and I really enjoyed this panel discussion. So I’m just going to have some closing remarks, and thank everyone for attending. Please let us know your thoughts about this event by responding to the short survey that’s going to be added as a link in the chat. I’ll also highlight that this video has been recorded and will be available on our YouTube channel. It will take about a week or two for closed captioning to be finalized, but if you have interest in revisiting any of these topics, you can find it there. You can also please visit UMServicetosociety.org to explore our strategic directions here at the University of Michigan. And we also have a new LinkedIn page with some information on it. So please feel free to explore that there.
Thank you all so much for attending, and this was absolutely fantastic and I am so happy that we had the opportunity to have this discussion and to really share these ideas because I think this is incredibly important moving forward. So, thank you.

Marketing Communications Specialist
Department of Civil and Environmental Engineering